The Centers for Medicare and Medicaid Services (CMS) issued its final rule updating Medicare payment policies for skilled nursing facilities (SNF) for fiscal year (FY) 2024 on July 31, 2023. These rules are effective October 1, 2023. Below is an overview of the FY 2024 SNF Prospective Payment System (PPS), including finalized changes and other relevant updates.
Key Finalized Changes
The finalized rule includes the following key changes:
- An estimated 4% net increase in Medicare Part A SNF payments
- Changes to the SNF Quality Reporting Program (QRP)
- Changes to the SNF Value-Based Purchasing (VBP) Program
There’s also a measure meant to improve staffing shortages in skilled nursing facilities (SNF) and changes to the constructive waiver process designed to alleviate administrative burdens.
Updates to SNF Payments
CMS estimates an overall increase in payments by 4%, or $1.4 billion, to SNFs for FY 2024, compared to the initial proposed estimate of 3.7%. This adjustment comes from a 3% SNF market basket increase in addition to a 3.6% market basket forecast error adjustment with approximately 0.2% productivity adjustment. These changes also reflect a negative 2.3% reduction ($789 million) from the Patient Driven Payment Model (PDPM) parity adjustment recalibration introduced last year.
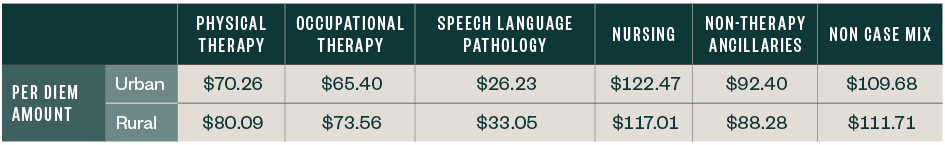
FY 2024 Unadjusted Federal Rate Per Diem
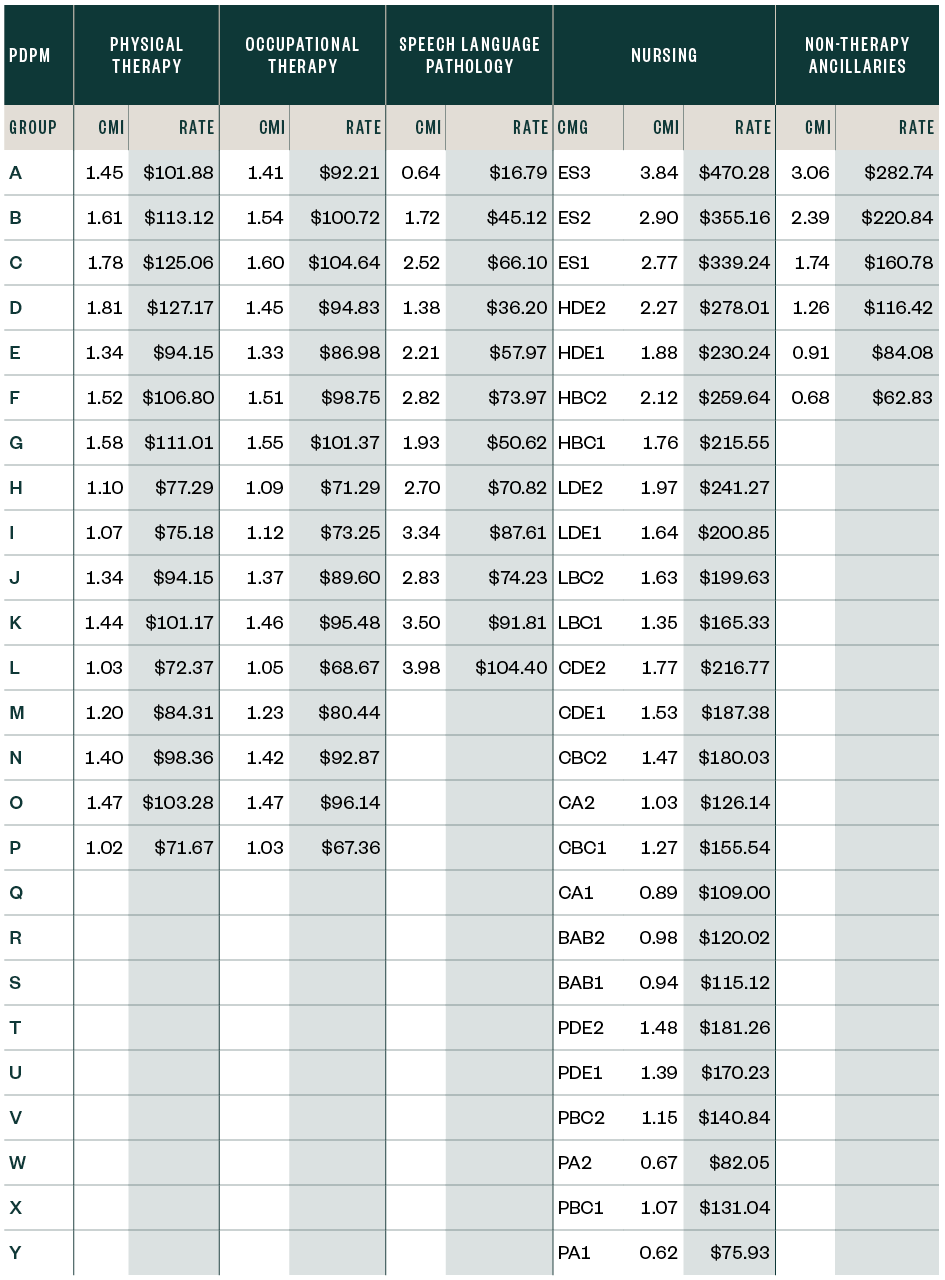
FY 2023 Unadjusted Federal Rate Per Diem

The chart below includes the second phase of the Parity Adjustment Recalibration.
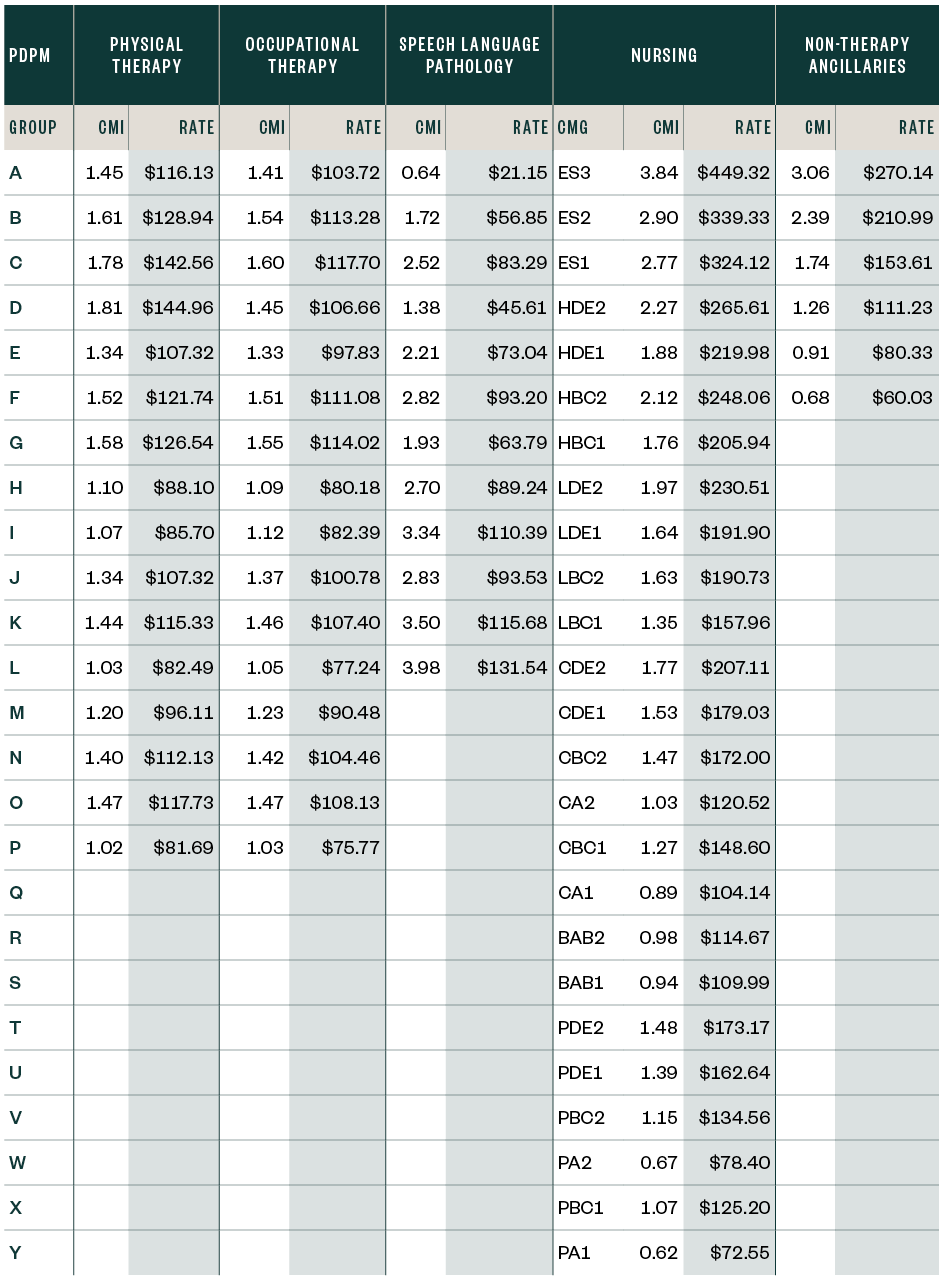
PDPM Case-Mix Adjusted Federal Rates and Associated Indexes—Rural
The chart below includes the second phase of the Parity Adjustment Recalibration.
SNF QRP
Under the new rule, SNFs that don’t meet reporting requirements will see a two percentage point reduction to their Annual Payment Update (APU).
CMS is adopting two new measures, modifying one, and removing three from the QRP. CMS is adding the Discharge Function measure starting in FY 2025. This measure assesses functional status by measuring the percentage of SNF residents that meet or exceed expected discharge functional scores, while utilizing mobility and self-care scores already included the Minimum Data Set (MDS).
CMS is also adopting a new measure reporting the percentage of stays in which residents are up to date with COVID-19 vaccinations according to the CDCs most recent guidance. This measure will be reported as a new standardized item on the MDS beginning in FY 2026.
In addition, CMS is modifying its measure tracking the percentage of healthcare personnel working in SNFs who are up to date with COVID-19 vaccinations according to the CDC. This measure previously only reported SNF personnel who had received the primary vaccination series.
SNF Value-Based Purchasing (SNF VBP) Program
The SNF VBP program currently includes all SNFs paid under Medicare’s SNF PPS and rewards facilities with incentive payments based on the quality of care provided. This final rule adopts new quality measures and finalizes several policy changes.
CMS is adding the Nursing Staff Turnover Measure beginning in FY 2026. This measure is publicly reported and assesses the stability of staffing within a facility. CMS reports this measure to be part of the commitment by President Joe Biden’s administration to ensure adequate staffing in long-term care facilities. Reporting begins in FY 2024 and payment impacts start in FY 2026.
Other new measures CMS is adopting include assessing the hospitalization rate of long-term residents—Long Stay Hospitalization Measure per 1,000 Days—and one to assess falls within facilities that result in major injuries for long-term residents. Both measures will be implemented beginning in FY 2027.
CMS is also adopting a Health Equity Adjustment to the SNF VBP program to reduce disparities in health care outcomes. This adjustment will reward high-performing SNFs where at least 20% of the patient population is dually eligible.
Civil Monetary Penalty Changes
CMS is adopting a constructive waiver process that considers a facility to have waived its hearing if it fails to request one within the required timeframe. This process, designed to alleviate administrative burden, will accompany a 35% penalty reduction already in place.
Next Steps
Providers need to review whether they’ve loaded appropriate SNF rates into the patient accounting system they use to bill Medicare on or after October 1, 2023.
Once the providers incorporate the revised rates, they can validate the rates are calculated appropriately. They can accomplish this by pulling a paid claim and running it through the SNF pricer, downloadable from the CMS website.
We’re Here to Help
For more information about the final rule and its implications, contact your Moss Adams professional.